Payal Saxena shares this video case “EUS-guided rendezvous and reversal of complete rectal anastomotic stenosis after Hartmann’s reversal.”
A 54-year-old man was found to have complete rectal anastomotic stenosis. He underwent left hemicolectomy, Hartmann’s pouch, and colostomy for management of ischemic colitis. Several months later he had Hartmann’s reversal and diverting loop ileostomy performed. Prior to reversal of the ileostomy, diagnostic colonoscopy revealed complete anastomotic stenosis.
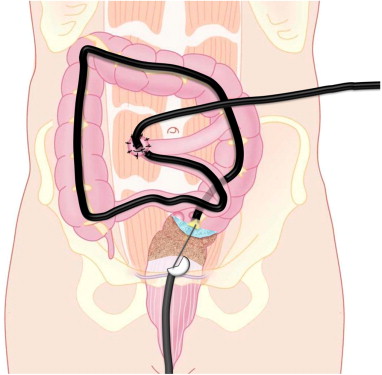
The patient underwent EUS guided reversal of the stenosis. A colonoscope was passed through the ileostomy to the proximal aspect of the stenosis. An echoendoscope was passed transanally to the distal aspect of the stenosis. The proximal colon was filled with water. Under EUS guidance, a 19g needle was passed across the stenosis into the proximal colonic lumen. A 0.025 inch guidewire was passed through the needle into the proximal colon. The stenosis was dilated over the wire using a 6mm balloon. A 10mm × 80mm fully covered self-expandable metallic stent was placed across the dilated tract. A double pigtail stent was placed through the metal stent to prevent migration. The patient returned 1 week later after spontaneous stent migration. The recto-colonic tract was widely patent. The patient returned weekly for sequential balloon dilatation to 15mm, 18mm, and 20mm. Follow-up barium enema revealed a completely patent recto-colonic fistula.
A 54-year-old man was found to have complete rectal anastomotic stenosis. He underwent left hemicolectomy, Hartmann’s pouch, and colostomy for management of ischemic colitis. Several months later he had Hartmann’s reversal and diverting loop ileostomy performed. Prior to reversal of the ileostomy, diagnostic colonoscopy revealed complete anastomotic stenosis.
The patient underwent EUS guided reversal of the stenosis. A colonoscope was passed through the ileostomy to the proximal aspect of the stenosis. An echoendoscope was passed transanally to the distal aspect of the stenosis. The proximal colon was filled with water. Under EUS guidance, a 19g needle was passed across the stenosis into the proximal colonic lumen. A 0.025 inch guidewire was passed through the needle into the proximal colon. The stenosis was dilated over the wire using a 6mm balloon. A 10mm × 80mm fully covered self-expandable metallic stent was placed across the dilated tract. A double pigtail stent was placed through the metal stent to prevent migration. The patient returned 1 week later after spontaneous stent migration. The recto-colonic tract was widely patent. The patient returned weekly for sequential balloon dilatation to 15mm, 18mm, and 20mm. Follow-up barium enema revealed a completely patent recto-colonic fistula.
Figure 1. A colonoscope is advanced through the ileostomy to the distal colon, to the level of the rectal anastomotic stenosis. The proximal colon is filled with water. An echoendoscope is seen in the rectum (passed through the anus) and a needle is advanced under EUS guidance across the anastomosis into the proximal colon.
This video demonstrates a very novel rendezvous technique. The only other management option for this patient was major surgery that was avoided, and we were able to provide a minimally invasive, endoscopic solution to the problem.
We were able to perform this procedure safely by combined use of EUS and fluoroscopic guidance. Most importantly, access to the proximal colonic lumen via the ileostomy enabled dual endoscopic views and added safety to the procedure.
This video demonstrates a very novel rendezvous technique. The only other management option for this patient was major surgery that was avoided, and we were able to provide a minimally invasive, endoscopic solution to the problem.
We were able to perform this procedure safely by combined use of EUS and fluoroscopic guidance. Most importantly, access to the proximal colonic lumen via the ileostomy enabled dual endoscopic views and added safety to the procedure.
 RSS Feed
RSS Feed
