Payal Saxena, MD, from Johns Hopkins University in Baltimore, Maryland writes about her Original Article titled “EUS-guided biliary drainage by using a standardized approach for malignant biliary obstruction: rendezvous versus direct transluminal techniques (with videos)” from the November issue.
The aim of this study was to assess outcomes of EUS-guided biliary drainage (EGBD) performed using a standardized approach in addition to comparing the outcomes of EGBD via the rendezvous technique (REN) or the direct transluminal technique (TL).
There has been growing international experience with EGBD. The current data suggests that severe adverse events are rare, however most series include a small number of patients. Also, there is no data comparing the REN and TL techniques of EGBD. The REN technique is performed by passing a wire across the papilla and is preferred by many endoscopists as it avoids the need for a permanent bilio-enteric fistual and need for dilatation of the fistulous tract which can lead to adverse events (bleeding, pneumoperitoneum, pneumomediastinum). However, the REN technique is not feasible if the papilla cannot be accessed due to altered anatomy or gastric outlet obstruction. The REN technique has also been associated with a risk of pancreatitis and lengthy procedural times attributed toward wire manipulation. The TL technique can be performed entirely transgastrically or transduodenally without accessing the papilla.
EGBD was performed with technical success in 94% (33/35) of patients, TL technique was used in 20 patients, and REN technique in 13. Clinical success was achieved in 97% (32/33) patients. Only 4 (12%) procedure related adverse events occurred, 2 mild (mild pancreatitis, limited pneumoperitoneum), 1 moderate (retained sheared wire), and 1 severe (acute cholecystitis). There was no statistically significant difference in clinical success, procedure time, adverse events, or length of hospital stay between the TL and REN groups.
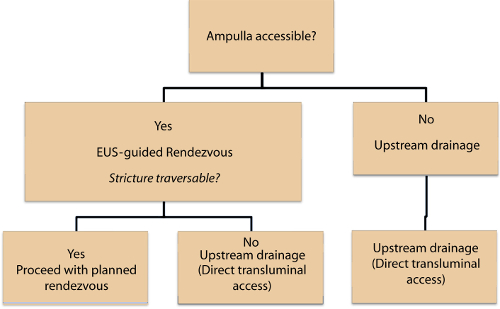
The TL technique has not been widely studied when compared to the REN technique. Our study shows the TL technique is safe and bile leak or pneumoperitoneum can be avoided with the use of metallic stents and carbon dioxide insufflation, respectively. Furthermore, the use of larger covered metallic stents results in complete seal of the iatrogenic bilioenteric tract, preventing bile leak. Our study demonstrates that use of a standardized approach (Figure 1) allows EGBD to be performed safely and effectively. Prospective, randomized trials are needed to compare the safety and efficacy of the TL and REN techniques of EGBD.
The aim of this study was to assess outcomes of EUS-guided biliary drainage (EGBD) performed using a standardized approach in addition to comparing the outcomes of EGBD via the rendezvous technique (REN) or the direct transluminal technique (TL).
There has been growing international experience with EGBD. The current data suggests that severe adverse events are rare, however most series include a small number of patients. Also, there is no data comparing the REN and TL techniques of EGBD. The REN technique is performed by passing a wire across the papilla and is preferred by many endoscopists as it avoids the need for a permanent bilio-enteric fistual and need for dilatation of the fistulous tract which can lead to adverse events (bleeding, pneumoperitoneum, pneumomediastinum). However, the REN technique is not feasible if the papilla cannot be accessed due to altered anatomy or gastric outlet obstruction. The REN technique has also been associated with a risk of pancreatitis and lengthy procedural times attributed toward wire manipulation. The TL technique can be performed entirely transgastrically or transduodenally without accessing the papilla.
EGBD was performed with technical success in 94% (33/35) of patients, TL technique was used in 20 patients, and REN technique in 13. Clinical success was achieved in 97% (32/33) patients. Only 4 (12%) procedure related adverse events occurred, 2 mild (mild pancreatitis, limited pneumoperitoneum), 1 moderate (retained sheared wire), and 1 severe (acute cholecystitis). There was no statistically significant difference in clinical success, procedure time, adverse events, or length of hospital stay between the TL and REN groups.
The TL technique has not been widely studied when compared to the REN technique. Our study shows the TL technique is safe and bile leak or pneumoperitoneum can be avoided with the use of metallic stents and carbon dioxide insufflation, respectively. Furthermore, the use of larger covered metallic stents results in complete seal of the iatrogenic bilioenteric tract, preventing bile leak. Our study demonstrates that use of a standardized approach (Figure 1) allows EGBD to be performed safely and effectively. Prospective, randomized trials are needed to compare the safety and efficacy of the TL and REN techniques of EGBD.
 RSS Feed
RSS Feed
